- Received February 24, 2021
- Accepted March 08, 2021
- Publication June 08, 2021
- Visibility 1 Views
- Downloads 0 Downloads
- DOI 10.18231/j.jooo.2021.022
-
CrossMark
- Citation
Bilateral nasolabial flap and Buccal fat pad flap for reconstruction of fibrotomy defect in surgical management of stage III/IV Oral Submucous Fibrosis (OSMF) – A comparative study
- Author Details:
-
Suneedh Gupta
-
Mohammad Ali R Patel *
-
Mohammed Haneef
-
Shakeel Ahmed
-
Juveria Arshi
Introduction
Oral submucous fibrosis may be defined as “An insidious precancerous chronic disease that may affect the entire oral cavity and sometimes extends to the pharynx. Although it is occasionally preceded by formation of vesicles; it is always associated with sub-epithelial inflammatory reaction that is followed by fibroelastic change of the lamina propria with epithelial atrophy. This leads to stiffness of the oral mucosa resulting in trismus and inability to eat.”[1], [2], [3], [4] It is predominantly seen in people in southern Asian countries or southern Asian immigrants to other parts of the world. However occasional cases have been reported in Europeans and people from Taiwan, China, Nepal, Thailand and Vietnam.[1], [5], [6]
Stage III/IV OSMF show minimal response at best to medicinal line of treatment, surgical release of fibrotic bands has been advocated to improve the mouth opening.[3], [7], [8]
Initially surgeons aimed at surgical elimination of the fibrotic bands which showed further scar formation and reoccurrence of trismus, hence to prevent they started using various inter positional grafts/flaps.[3], [7], [8] A variety of grafts/flaps have been documented cover to heal denuded areas and surgical defects in an attempt to find the ideal graft/flap cover.[3], [8], [9], [10] Additional procedures like extraction of third molars, bilateral coronoidotomy, masticatory myotomy have also been documented to enhance mouth opening have also been advocated.[10]
Aim and Objectives
To evaluate and compare the effectiveness of two reconstructive modalities, i.e., B/L Buccal Fat Pad (BFP) and B/L single stage Nasolabial Flap (NLF) for the reconstruction of the defects in buccal mucosa, secondary to fibrotomy in surgical management of oral submucous fibrosis Stage III/IV The objectives of the study are:
Evaluate the Maximum Inter-Incisal Opening (MIO) distance as an objective criterion intraoperatively and 6 months post operatively and compare them statistically.
Statistically comparing the post-operative Surgical Complications between the two flap choices; Three common parameters were selected i.e., Perforation/dehiscence, sloughing and infection.
Materials and Methods
This is a multi-center study and patients were selected as per Inclusion and Exclusion criteria. The patients were divided into two groups i.e., Group A and Group B. B/L Nasolabial Flap was used for Group A and B/L BFP was used for Group.
Inclusion criteria
Medically fit Male Patients without history of past surgical/medical intervention.
Patients who have confirmed to have stopped the habit for 6 months or more.
Patients with clinically confirmed with Stage III/IV OSMF3
Patients who consented to surgical intervention with either use of NLF / BFP to cover the fibrotomy defect and use of the data for academic interest.
Patients who underwent physiotherapy and post-operative follow-up for 6 months.
Exclusion criteria
Patients who had additional habits like alcohol abuse, smoking etc in addition to betel quid chewing.
Heavy facial hair growth.
Scarring from previous insult or treatment.
All surgical procedures were performed under general anesthesia using fibro-optic intubation technique. The Stenson’s duct orifice was identified and marked B/L to prevent any injury to it. The intraoral incisions were made bilaterally at the level of occlusal plane, away from the Stenson’s duct orifice on each side of the buccal mucosa using electrosurgical knife. Bilaterally incisions were extended posteriorly to the pterygomandibular raphe or anterior faucial pillar and anteriorly to the corner of mouth depending on the location of fibrous bands. B/L fibrotomy was done and further undermining was done by blunt dissection until no resistance was felt. B/L Coronoidotomy and myotomy was relieving the insertions temporalis medial pterygoid and originating fibres of masseter muscle with the coronoid process. All third molar teeth were extracted as required. Intraoperative forced mouth opening. The mouth was then forced open using Fergusson’s mouth gag to achieve maximum MIO. Mean intra-operative mouth opening achieved was an avg of 41mm. The dimensions of the resultant soft tissue defects created averaging about 2.25 cm in width and and 5.5 cm in lenght.
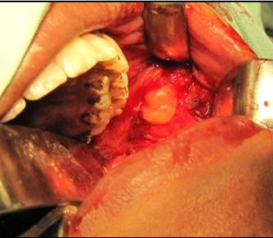
Group A: The buccal fat pad was approached bilaterally via the posterior superior margin of the created buccal soft tissue defect through a tunnel along the ascending ramus of mandible and from the lateral surface of buccinator muscle by gentle dissection and lateral pressure on the cheek ([Figure 1]). The buccal fat pad flap was then pulled out gently until a sufficient amount was obtained to cover the defect without tension. The buccal fat pad covered the buccal defect posteriorly to the soft palate and anteriorly to the corner of mouth. The flap was then secured in the place by horizontal mattress suturing technique using 3-0 resorbable sutures (Polyglactin 910-Vicryl) ([Figure 2]).

Group B: Inferiorly based single stage nasolabial flap was designed and marked bilaterally on the skin of the nasolabial region ([Figure 4]). The facial artery was identified beneath the skin with the assistance of its anatomical landmarks. The base of the flap was about 1.5-2.0 cm in width and its length was about 5-7 cm. The base of the flap was maintained just above the corner of the mouth to avoid injuries to the branches of facial artery & inferior labial artery; which pass into nasolabial skin and subcutaneous tissue. The flap was marked superiorly in elliptical fashion with medial and lateral limbs of the flap tapering 2-2.5 cm antero-inferiorly from the medial canthus of the eye.


The flap was raised from superior to inferior direction with sufficient enough subcutaneous tissue to provide a good blood supply, but remained superficial to the facial muscles. The base of the flap was maintained just above the level of the angle of mouth. A trans buccal tunnel was made at the level of the angle of mouth using Metzenbaum scissors ([Figure 5]). The width of the tunnel was kept at least as wide as or slightly wider than the flap width. The flap was transferred into the oral cavity in a tension free manner and inset into the defect by horizontal mattress suturing technique using 3-0 resorbable sutures (Polyglactin 910-Vicryl). The cutaneous surface of the flap in the region of the modiolus was de-epithelized to eliminate the need for pedicle division after 3 weeks. The flap was then transferred into the oral cavity in a tension free manner. Intraorally, the flap was sutured by placing interrupted resorbable sutures ([Figure 6]). The donor site was undermined in subcutaneous plane as skin lift rhytidectomy and closed in layers. An attempt was made to evert the skin along the nasolabial portion of the incision to achieve a flat or depressed scar which results in a natural appearance. Dressing was done using paraffin impregnated Tulle-Grass (Cuticell).




Postoperative follow up protocol:
All patient were kept on nasogastric tube feeding for duration of 10 days.
The patients were given with IV antibiotics for a period of 5 days followed by oral antibiotics for another 5 days. Thorough irrigation with povidone iodine 5% solution, saline and Chlorhexidine Gluconate 0.2% w/v was done twice a day for the postoperative period of about 15 days.
Extraoral sutures were removed on 7th post-operative day in cases of nasolabial flap. On 15th post-operative day, all intra oral sutures were removed.
Aggressive Physiotherapy was started from first Post-op day onwards using heisters jaw opener, for half an hour initially. Later the duration and frequency of exercise was increased for further improvement in mouth opening, until satisfactory result was achieved.
Patients were evaluated for complications and maximum incisal opening (MIO) was recorded at intervals of14th day, 1st month, 3rd month and 6th months post operatively but comparison was done at 6 months.
All patients were prescribed nutrient supplement and anti-oxidant capsules of[10] Lycopene 5000mcg once daily with topical triamcinolone acetonide 0.1% on mucosal surface at bedtime for minimum of 6 months postoperatively.
Results
The mean pre-operative inter-incisal distance was 12.80 mm with (SD-3.120) in Group A and 12.30 mm (SD-2.983) in Group B. ([Table 1])
Intra operatively 40.90mm with (SD-4.228) in Group A and in Group B it was 41.10 with (SD-1.449) ([Table 1]). At the end of 6 months of post-operative follow-up group A & group B had achieved statistically significant mean mouth opening of 31.90 mm (SD-4.458) & 29.20 mm (SD-1.687) ([Table 2]); no significant differences were seen in mean interincisal mouth opening using student “t” test) (p <0.05) ([Table 1]) with statistically significant Net gain of 19.10 in Group A Net gain of 16.90 in Group B ([Table 2]).
|
Groups |
|
Mean |
Std. Deviation |
Std. Error Mean |
t value |
P value |
|
|
Pre-operative |
Group A |
10 |
12.80 |
3.120 |
.987 |
.366 |
.718 |
|
Group B |
10 |
12.30 |
2.983 |
.943 |
|||
|
Intra operatively |
Group A |
10 |
40.90 |
4.228 |
1.337 |
.141 |
.889 |
|
Group B |
10 |
41.10 |
1.449 |
.458 |
|||
|
6 months Post-operatively |
Group A |
10 |
31.90 |
4.458 |
1.410 |
1.791 |
.090 |
|
Group B |
10 |
29.20 |
1.687 |
.533 |
|
Group A |
Group B |
|||
|
Mean |
Std. Deviation |
Mean |
Std Deviation |
|
|
Preop |
12.8 |
3.12 |
12.30 |
2.98 |
|
6mo |
31.90 |
4.45 |
29.20 |
1.68 |
|
Net gain |
19.10 |
2.37 |
16.90 |
2.64 |
|
t value |
25.39 |
20.21 |
||
|
P value |
<0.0001* |
<0.0001* |
Post-operatively in Group A one patient had got perforation/dehiscence in flap which had been re-sutured, two flaps had got infected ([Table 4]). Epithelization of BFP started from 2nd week onwards completed within 3-4 weeks.
Post-operatively in Group B ([Table 4]) three patients had got infection and one patient developed subsequent oro-cutaneous fistula of the flap which were treated by systemic antibiotics. Two patients had got sloughing of the flap at the margins which was managed by gentle debridement and irrigation with Povidone Iodine 5% solution. Two patients had got intraoral hair growth which was treated by laser. Extraoral healing was uneventful in all cases except the patient who had developed oro-cutaneous fistula. Extraoral scars were perceptible and comparable in all patients in Group B except the one patient who was diagnosed with oro-cutaneous fistula further developing pin cushion effect. We did not record any complaint of widening of oral commissure. Mucolisation of the NLF took to between 4 to 6 months, it was delayed in patient who had intra-oral hair growth.
No statistically significant difference was seen in number complications in both study groups when compared using Fischer exact test as p>0.05 ([Table 5]).
|
Groups |
|
Mean Net Gain |
Std Deviation |
Std. Error mean |
t value |
P value |
|
|
Net gain |
Group A |
10 |
19.1000 |
2.37814 |
.75203 |
1.956 |
0.66 |
|
Group B |
10 |
16.9000 |
2.64365 |
.83600 |
|
Complications |
Total |
|||||
|
Perforation |
Sloughing |
Infection |
||||
|
Groups |
Group A |
N-10 |
1 |
0 |
2 |
3/10 |
|
Group B |
N-10 |
0 |
2 |
3 |
5/10 |
|
Complications |
Total |
||||
|
No |
Yes |
||||
|
Groups |
Group A |
7 |
3 |
10 |
|
|
% |
70.0% |
30.0% |
100.0% |
||
|
Group B |
5 |
5 |
10 |
||
|
% |
50.0% |
50.0% |
100.0% |
||
|
Total |
12 |
8 |
20 |
||
|
% |
60.0% |
40.0% |
100.0% |
||
|
P value |
0.325 |
Discussion
Sushruta had described Oral submucous fibrosis in Indian literature as “VIDARI”.[6] In modern literature, it was first described by Schwartz in 1952; among 5 Indian women from Kenya and he called “atrophia idiopathica mucosae oris”.[6] Later it was called as Oral submucous fibrosis.[11] Surgical treatment of severe trismus in submucous fibrosis patients can improve articulation, mastication, and oral hygiene, which are socially and functionally important.[12], [13]
Initially surgeons aimed at surgical elimination of the fibrotic bands which showed further scar formation and reoccurrence of trismus, hence to prevent they started using various inter positional grafts/flaps material.[12], [4]
Buccal fat pad was first identified by Lorenz Heister in 1732[11] and since extensive of use of it for local reconstruction of defects has been documented. Buccal fat pad by virtue of its anatomic position and the ease with which it can be accessed and mobilized without causing any noticeable defect in the cheek or mouth was felt to be reliable inter-positional material. The flap can be approached through the same buccal incision which was used to release the fibrous bands. On an average, the volume of BFP is 9.6 mL (range, 8.3 - 11.9 mL in length).[11], [14] Defects measuring up to 3 to 5 centimetres (cm) can be safely covered[14] without any surgical consequence and lasting effects in a single stage procedure. The main limitation of the buccal pad of fat is its limited size which may require additional graft/flap for coverage of defect.
The subcutaneous pedicled nasolabial flaps have been originally described 2500 years ago in the works of Sushruta in 600 BC,[12] and its use for reconstruction has also been documented.
The nasolabial flap is a random pattern flap based on the subcutaneous blood supply from the transverse facial and angular branches of the facial artery. Large flap can be safely harvested which can effectively cover both posterior and anterior fibrotomy. Its disadvantages include, technical skill, need of flap division/de-epithelisation, infection, minor or major flap necrosis, wound dehiscence, Asymmetry at the level of the nasolabial fold is noted if proper suturing is not done, extra-oral scarring, pin cushion effect, loss of nasolabial fold and widening of oral commissure giving fish mouth appearance which can require surgical correction.
Our study results contrast and are reverse of the results reported by Rai et al. (2014); they reported the postoperative mouth opening in Group I (NLF) was 32 mm respectively, while in Group II (BFP) the values were 29 mm respectively at 1 year follow up. The pre-operative recorded mean MIO was 10mm (NLF) and 12mm (BFP), while in our study it was 12.30 mm and 12.80 mm each respectively. They also report of higher complications in the NLF group. The most common immediate complication in both the groups was subluxation and delayed complication was Fish mouth in NLF group.
Our study results are in accordance to the results achieved by Aggarwal et al. (2018); they reported microtomy no statistically difference in mean MIO between BFP and NLF at 6 months period which concurs our study. They reported significant Net gain MIO in NLF group which is in contrast to our result.
Bhujpal PV et al. (2019) conducted systematic review and reported that the choice of procedure seems to be determined entirely by the preference of the surgeon. This review also reported that buccal fat pad offers better interincisal opening than nasolabial flap which is in contrast to our study where we found no significant difference between the two at 6 months post-operatively.
Anehosur V et al. (2020) The mean preoperative and postoperative interincisal mouth opening was 12 mm and 27 mm in group I (BFP) and 11 mm and 38 mm in group II(NLF) at 1-year post-operative follow up which is in contrast to our study. Their reported proposed surgical protocol for the management of OSMF found NLF superior to BFP for the reconstruction of intraoral defects after the release of fibers in patients with OSMF, with a minimal residual scar.
Tiwari P et al. (2020) reported a systemic review, of three of the five studies selected in review favoured buccal fat pad over nasolabial flap because of its ease of harvest and reduced number of post-operative complications. One study favoured nasolabial flap because of the progressive increase in mouth over opening and amount of the tissue obtained for reconstruction. However, they have reported a general consensus has been towards favouring buccal fat pad over nasolabial flap.
Conclusion
We conclude that both NLF and BFP are viable reconstruction methods; however, we propose the use of single stage NLF in case of extensive disease where BFP may not viable method of reconstruction. As the flap cannot cover the larger post fibrotomy defect. Additionally, BFP flap in our view is marginally more preferable due to ease of harvesting, patient acceptance, decreased rate of complications and lasting surgical effect.
This study limited by sample size and short-term follow-up period. An extensive clinical trial with a greater number of cases, with increased number of parameters is necessary to come final conclusion with respect to long term post-operative mouth opening.
Also, the importance of post-operative physiotherapy, strict patience compliance and cessation of habit are key to successful outcome in treatment of late stage OSMF.
Source of Funding
None.
Conflict of Interest
The authors declare that there is no conflict of interest.
References
- SM Haider, AT Merchant, FF Fikree, MH Rahbar. Clinical and functional staging of oral submucous fibrosis. Br J Oral Maxillofac Surg 2000. [Google Scholar] [Crossref]
- DK Paissat. Oral submucous fibrosis. Int J Oral Surg 1981. [Google Scholar] [Crossref]
- JN Khanna, NN Andrade. Oral submucous fibrosis: a new concept in surgical management. Int J Oral Maxillofac Surg 1995. [Google Scholar] [Crossref]
- DR Lai, HR Chen, LM Lin, YL Huang, CC Tsai, DR Lai. Clinical evaluation of different treatment methods for oral submucous fibrosis. A 10-year experience with 150 cases. J Oral Patho Med 1995. [Google Scholar] [Crossref]
- NM Kavarana, HM Bhathena. Surgery for severe trismus in submucous fibrosis. Br J Plast Surg 1987. [Google Scholar] [Crossref]
- RM Borle, SR Borle. Management of oral submucous fibrosis: A conservative approach. J Oral Maxillofac Surg 1991. [Google Scholar] [Crossref]
- DJC Yen. Surgical treatment of submucous fibrosis. Oral Surg 1982. [Google Scholar]
- MC Kothari, N Hallur, B Sikkerimath, S Gudi, CR Kothari. Coronoidectomy, masticatory myotomy and buccal fat pad graft in management of advanced oral submucous fibrosis. Int J Oral Maxillofac Surg 2012. [Google Scholar] [Crossref]
- D Mehrotra, R Pradhan, S Gupta. Retrospective comparison of surgical treatment modalities in 100 patients with oral submucous firbosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009. [Google Scholar]
- X Jiang, J Hu. Drug Treatment of Oral Submucous Fibrosis: A Review of the Literature. J Oral Maxillofac Surg 2009. [Google Scholar] [Crossref]
- R Rajendran. Oral submucous fibrosis: etiology, pathogenesis, and future research. Bull World Health Organ 1994. [Google Scholar]
- Y Ducic, M Burye. Nasolabial flap reconstruction of oral cavity defects: A report of 18 cases. J Oral Maxillofac Surg 2000. [Google Scholar] [Crossref]
- R Rajendran. Oral submucous fibrosis: etiology, pathogenesis, and future research. Bull World Health Organ 1994. [Google Scholar]
- A Rai, A Datarkar, M Rai. Is buccal fat pad a better option than nasolabial flap for reconstruction of intraoral defects after surgical release of fibrous bands in patients with oral submucous fibrosis? A pilot study: A protocol for the management of oral submucous fibrosis. J Cranio-Maxillofac Surg 2014. [Google Scholar] [Crossref]
